Delivery
What are possible labor complications?
Serious complications are rare during labor. But some problems can happen during this time. Some of the more common ones are listed below.
Fetal meconium
When the amniotic sac ruptures, the normal color of the amniotic fluid is clear. But if the fluid is greenish or brown in color, it may show fetal meconium. This is normally passed after birth as the baby's first bowel movement. Meconium in the amniotic fluid may be linked to fetal distress. Talk with your healthcare provider right away.
Abnormal fetal heart rate
The fetal heart rate during labor is a good sign of how the fetus is handling the contractions of labor. The heart rate is usually kept track of electronically during labor. The normal range varies between 120 and 160 beats per minute. If the heart rate shows that a fetus may be in trouble, action can be taken right away. You can get oxygen and more fluids. You can also change your position.
Abnormal position of the fetus during birth
The normal position for the fetus during birth is head-down, facing your back. But sometimes a fetus is not in the right position. This may make delivery harder through the birth canal. There are several abnormal positions for a fetus:
-
Positioned head-down but facing your front
-
Positioned with the face down into your pelvis, instead of the top of the fetal head
-
Positioned with the brow down in your pelvis
-
Positioned breech. This means the buttocks or feet are down first in your pelvis.
-
Positioned with one shoulder in your pelvis
Depending on the position, a healthcare provider may try to deliver the fetus as it presents itself. Or the provider may try to turn the fetus before birth, or do a C-section (cesarean delivery).
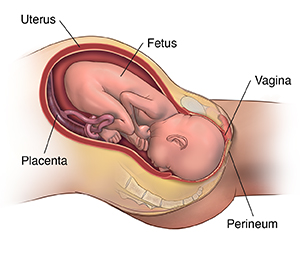
Delivery of the baby
Delivery is the moment when the fetus and the placenta leave your body. To get ready for the delivery, you may be moved into a birthing room or delivery room. Or you may stay in the same room for both labor and the birth. Fathers or partners are encouraged to be actively involved in childbirth by helping with relaxation methods and breathing exercises.
Positions for delivery may vary from squatting, sitting, to semi-sitting positions (between lying down and sitting up). With semi-sitting positions, gravity can help you push the baby through the birth canal. The type of position for birth depends on your preference and your healthcare provider's. It also depends on the health of the fetus.
During the delivery process, the healthcare staff will continue to keep an eye on your blood pressure, pulse, and other vital signs, and the fetal heart rate. The healthcare provider will check the cervical opening to see the position of the fetus' head. They will continue to support and guide you in your pushing efforts.
Delivery can be done either vaginally or by C-section.
What is a vaginal delivery?
During a vaginal delivery, the healthcare provider will help the fetus's head and chin out of the vagina when it becomes visible. Once the head is delivered, the healthcare provider puts gentle downward traction on the head to deliver the shoulder. The rest of the body follows. The baby turns itself as the last movement of labor.
In some cases, the vaginal opening does not stretch enough to fit the fetus. Delivery may need to be sped up. This might be needed if the baby is in distress. In such cases, the healthcare provider may do an episiotomy. This is a cut through the vaginal wall and the perineum. The perineum is between the thighs, extending from the anus to the vaginal opening. An episiotomy is done to help deliver the fetus. Episiotomies are not needed for every birth. They are not routinely done.
After the birth of the baby, you will be asked to continue to push during the next few uterine contractions to deliver the placenta. Once the placenta is out, the provider will fix any tear or episiotomy. You often will be given oxytocin. This is by shot into the muscles or as an IV. This medicine is used to contract the uterus. The uterus is then massaged to help it contract. This also helps prevent too much bleeding.
What is a C-section?
If you aren't able to deliver the fetus vaginally, the fetus is delivered in surgery with a cesarean section. These are often done in an operating room or a designated delivery room. Some C-sections are planned and scheduled. Others may be done because of problems that occur during labor.
Once the anesthesia has taken effect, the provider makes a cut in the abdomen (belly) and makes an opening in the uterus. The amniotic sac is opened, and the baby is delivered through the opening. You may feel some pressure, a pulling sensation, or both.
After the birth of the baby, the healthcare provider will stitch the uterus and the cut that was made in the abdomen. After a C-section or vaginal delivery, you will have some bleeding.
Conditions for a C-section
Several conditions may make having a baby by C-section more likely. These are:
-
Previous C-section
-
Fetal distress
-
Abnormal birth position, such as breech, shoulder, or face
-
A labor that fails to progress or doesn't progress normally
-
Placental problems, such as placenta previa. This is when the placenta blocks the cervix. It raises the risk that the placenta will become detached too soon from the uterus.
-
Twins or other multiples